GERD (Gastroesophageal Reflux Disease) is common during pregnancy, affecting 17-45% of all pregnant women. This article focuses on the natural treatment of GERD during pregnancy. It covers diet and lifestyle modifications, natural antacids (calcium & magnesium), digestive enzymes, probiotics, herbal medicines, and conventional medicines. Because conventional medication is sometimes required, there’s a section about how to minimize the side effects and nutrient deficiencies that may arise as a result of consuming an acid-suppressing medication.
What Is GERD?
GERD is an acronym for gastroesophageal reflux disease and is also known as reflux, acid reflux, and heartburn. GERD may be a digestive disease, but it affects all aspects of life, including emotional state, sleep, eating and drinking, and physical and social functioning.
When someone has GERD, the valve that keeps the contents of the stomach separate from the esophagus doesn’t close properly. This valve is called the lower esophageal sphincter and safely keeps stomach acid and digestive enzymes in the stomach. When the lower esophageal sphincter doesn’t close properly, acidic stomach contents can reflux back up into the esophagus.
GERD symptoms include burning pain in the upper abdomen or chest after meals, burning pain that may be worse in the evening or when lying down, sensation of a lump in the throat, difficulty swallowing, regurgitation of food or sour liquid, sour taste in the mouth, nausea and/or vomiting, chronic cough, hoarse voice, bloating, burping, frequent hiccups, and chronic sore throat.
What Causes GERD During Pregnancy?
The causes of GERD are complex and include insufficient lower esophageal sphincter tone, hiatal hernia, and food intolerances.
Insufficient lower esophageal sphincter tone or strength is a significant contributing factor to the development of GERD during pregnancy. This is especially true of GERD which develops during the last trimester and/or GERD that is worsened by eating large meals. Both increase the amount of pressure in the stomach and on the lower esophageal sphincter.
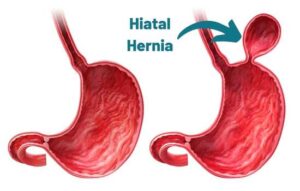
A hiatal hernia occurs when part of the stomach bulges up above the diaphragm. This can cause or worsen GERD symptoms. Pregnancy may also increase the chances of hiatal hernia because it increases abdominal pressure, which may lead to the stomach being pushed up and out of place.
Food allergies and intolerances are implicated in many cases of GERD. However, during pregnancy, I don’t usually recommend an elimination diet as I do at other times. I find that it works better for pregnant women to keep a food diary and to note which foods cause reflux symptoms.
Medications And Supplements That Cause Or Worsen GERD
Some medications, herbs, and supplements may cause or worsen reflux symptoms. Before working on treating reflux, it is sometimes easier to remove the cause.
Medications that may worsen GERD:
- Blood pressure medications
- Antibiotics
- Antidepressants
- Anti-anxiety medications
- Pain relievers
Please don’t stop taking any prescription medication listed here without speaking with your physician first. Different forms of medications or alternatives may be available.
Herbs that may cause or worsen GERD:
- Spearmint
- Peppermint
- Ginger
- Fennel
- Lemon Balm
- Catnip
You’ll notice that herbs that may worsen GERD are also common treatments for stomach complaints. For example, ginger is a safe and effective treatment for nausea and vomiting during pregnancy AND it can also be used to treat GERD because it increases the rate at which food moves out of the stomach. Ginger is a first-line GERD treatment in my practice. However, it’s important to know that it may not be the right treatment for everyone.
Supplements that may cause or worsen GERD:
- Some forms of iron and zinc
- Some forms of vitamin C
- High doses of vitamin B6
Lifestyle Modifications To Reduce GERD
Diet and lifestyle modifications are important first steps in the treatment of GERD. Many people avoid having to take additional supplements or medications by making some or all of the following changes.
- Eat smaller portions more often rather than large meals
- Take a digestive enzyme with meals that are high in protein and/or fat
- Eat more green vegetables
- Elevate your head with an extra pillow or two at night
- Avoid lying down for at least 1-2 hours after eating
- Eat your last meal at least 3 hours before bed and avoid eating late at night
- Wear loose clothing around your waist to avoid increasing abdominal pressure
- Quit smoking
Identification Of Foods That Worsen Reflux
Some foods are more likely to cause reflux than others and they vary from person to person. One study found that 91% of people with GERD were intolerant to 5 or more foods!

If you’re able to identify which foods cause reflux for you, you can take steps to avoid the food altogether, reduce your intake of the food, or take digestive enzymes or antacids with the food to prevent symptoms.
Keep a food diary for two weeks to determine which foods cause or worsen reflux. Record the food that you eat, the drinks you consume, the time consumed, the portion size, and the symptoms that you experience along with their intensity on a scale of 1-10.
Foods that frequently cause reflux symptoms include onions, garlic, tomatoes, gluten, dairy, chocolate, peppermint, caffeine, alcohol, spicy foods, and fatty foods.
Read more about food intolerance: 21 Different Types of Food Sensitivities – Dr. Green Mom
Calcium And Magnesium For Natural Treatment of GERD During Pregnancy
Liquid calcium and magnesium supplements are my number one natural treatment for GERD during pregnancy. Calcium and magnesium are both soothing antacids that work by directly neutralizing stomach acid. Calcium and magnesium are also beneficial for both mom’s and baby’s overall health.
Keep an eye on the upper limits for calcium and magnesium supplementation during pregnancy because taking too much can have adverse effects. Remember to check the amounts that you’re getting in your prenatal vitamin, too.
The upper limit for supplemental calcium intake is 2,500 mg per day.
The upper limit for supplemental magnesium intake is 350 mg per day.
Probiotics Reduce Reflux
Probiotics can be used to reduce the symptoms of GERD, including nausea, belching, burping, and abdominal pain. One study of probiotic use in pregnant women found that using a multi-strain probiotic for four weeks reduced or eliminated reflux symptoms in the majority of women.
For best results, take probiotics with lunch and dinner for at least four weeks. Stopping probiotics may cause reflux to return; therefore, it may be necessary to continue taking probiotics for the full pregnancy. The good news is that taking probiotics has other benefits during pregnancy, including reducing the chances of testing positive for group B strep at 36 weeks, preventing gestational diabetes, and reducing perinatal anxiety and depression.
Herbal Medicine To Soothe Reflux

Many herbs can be helpful for soothing reflux; however, not all of them are safe during pregnancy.
My favorite pregnancy-safe herb for soothing reflux is marshmallow (althea officinalis). I prefer it as a glycerite or tea so that it can coat the esophagus, but marshmallow root can also be effective in capsule form.
Dandelion root, hawthorn berries, ginger, and turmeric are other herbs to consider for natural treatment of GERD during pregnancy.
Manual Therapy For GERD During Pregnancy
In my practice, I’ve found that various manual therapies can help reduce or eliminate GERD symptoms in pregnant women. Helpful therapies include chiropractic, visceral manipulation, and osteopathy. It’s important to find a practitioner who is comfortable working with pregnant women and who is skilled at treating digestive concerns.
Conventional Medications For GERD During Pregnancy
Conventional treatment, like natural treatment of GERD during pregnancy focuses on the implementation of the lifestyle modifications listed above. The safest treatments are considered to be calcium and magnesium-based antacids and alginic acid (eg. Gaviscon). Alginic acid is derived from seaweed and makes the top part of your stomach contents non-acidic so that if reflux occurs it isn’t painful.
Some antacids contain aluminum (eg. Mylanta). Conventional thought is that aluminum-containing antacids are safe during pregnancy, but I am not convinced and don’t recommend them.
If the above medications aren’t effective, acid-suppressing drugs (H2 blockers and proton pump inhibitors) may be used.
Ranitidine (Zantac) used to be a preferred heartburn treatment in pregnancy, but in 2019 it was recalled due to contamination with a carcinogen. There is now a new Zantac, with a different active ingredient, famotidine. Famotidine is also the active ingredient in Pepcid. These drugs are called H2 blockers and they are considered likely safe in pregnancy. If H2 blockers aren’t effective, proton pump inhibitors, other than omeprazole, may be considered.
Supplements To Consider If Using Conventional Medications For GERD
Both H2 blockers and proton pump inhibitors have the potential to cause nutrient depletion. This is critical to note during pregnancy when you need all the nutrients that you can get!
Protein is required for your developing baby and acid is required to break down protein into absorbable amino acids. In my practice, if a woman needs a conventional antacid to manage GERD during pregnancy, I recommend supplementation with a hydrolyzed protein powder or hydrolyzed collagen powder. Hydrolyzed means that it is already broken down.
Vitamin B12 and iron require acid to be liberated from food so that they can be absorbed. In my practice, pregnant women on acid-suppressing drugs need to have their vitamin B12 and iron levels monitored and I often have them take a sublingual vitamin B12 supplement and a gentle iron supplement.
In addition, H2 blockers can deplete folic acid, calcium, iron, and vitamin D. Proton pump inhibitors can deplete magnesium. You may get adequate amounts of these nutrients from your prenatal multivitamin and diet or you may need additional supplementation. Speak with your healthcare provider for guidance about how to work with nutrition, natural treatment, and conventional treatment of GERD during pregnancy.
Side Effects Of Acid-Suppressing Drugs
Proton pump inhibitors may increase the risk of contracting Covid-19 and other viral illnesses. For more information about treating Covid-19 while pregnant, see this article: Covid-19 Home Treatment When Pregnant. What Is Safe And What Isn’t? – Dr. Green Mom.
Exposure to acid-suppressing drugs (proton pump inhibitors or H2 blockers) is associated with the development of childhood asthma. Recent studies found that any exposure to acid-suppressing drugs increased the odds of asthma in toddlers by 85% and exposure for more than 14 days increased the odds of asthma in toddlers by 156%. The risk seems to be higher if the mom also has asthma.
In addition to asthma, children exposed to acid-suppressing drugs in the womb have a higher risk of developing allergic rhinitis, eczema, and multiple allergic diseases.
More research is needed to understand why acid-suppressing drugs increase the risk of infection and allergic disease. However, I hypothesize that an acidic stomach environment is needed for optimal immune function and microbiome composition. To counter these risks, I make sure that patients on acid-suppressing drugs are also on a good probiotic, and I often recommend an immunomodulating supplement to help keep the immune system balanced and to protect against infection. Postnatal supplementation with a specially formulated probiotic may help prevent the development of allergic diseases like eczema and asthma.
Summary
GERD is a digestive reflux condition that affects many pregnant women. Natural treatment of GERD during pregnancy focuses on improving digestion, probiotic support, lifestyle modifications, manual therapy, calcium and magnesium antacids, and soothing herbal treatments. Sometimes conventional treatment may be necessary; in which case, it’s important to remember that acid suppressing medications may cause nutrient depletion, most notably protein, iron, and vitamin B12. Acid suppressing medications seem to disrupt the gastric immune system, so extra care may be needed to provide optimum health for mom and baby.
References:
Cheng, J., & Ouwehand, A. C. (2020). Gastroesophageal Reflux Disease and Probiotics: A Systematic Review. Nutrients, 12(1), 132. https://doi.org/10.3390/nu12010132
Homayouni, A., Bagheri, N., Mohammad-Alizadeh-Charandabi, S., Kashani, N., Mobaraki-Asl, N., Mirghafurvand, M., Asgharian, H., Ansari, F., & Pourjafar, H. (2020). Prevention of Gestational Diabetes Mellitus (GDM) and Probiotics: Mechanism of Action: A Review. Current diabetes reviews, 16(6), 538–545. https://doi.org/10.2174/1573399815666190712193828
Desai, V., Kozyrskyj, A. L., Lau, S., Sanni, O., Dennett, L., Walter, J., & Ospina, M. B. (2021). Effectiveness of Probiotic, Prebiotic, and Synbiotic Supplementation to Improve Perinatal Mental Health in Mothers: A Systematic Review and Meta-Analysis. Frontiers in psychiatry, 12, 622181. https://doi.org/10.3389/fpsyt.2021.622181
Caselli, M., Zuliani, G., Cassol, F., Fusetti, N., Zeni, E., Lo Cascio, N., Soavi, C., & Gullini, S. (2014). Test-based exclusion diets in gastro-esophageal reflux disease patients: a randomized controlled pilot trial. World journal of gastroenterology, 20(45), 17190–17195. https://doi.org/10.3748/wjg.v20.i45.17190
Caselli, M., Lo Cascio, N., Rabitti, S., Eusebi, L. H., Zeni, E., Soavi, C., Cassol, F., Zuliani, G., & Zagari, R. M. (2017). Pattern of food intolerance in patients with gastro-esophageal reflux symptoms. Minerva medica, 108(6), 496–501. https://doi.org/10.23736/S0026-4806.17.05379-4
Sfara A, Dumitrascu DL. The management of hiatal hernia: an update on diagnosis and treatment. Med Pharm Rep. 2019 Oct;92(4):321-325. doi: 10.15386/mpr-1323. Epub 2019 Oct 25. PMID: 31750430; PMCID: PMC6853045.
Tadić, V. M., Dobrić, S., Marković, G. M., Dordević, S. M., Arsić, I. A., Menković, N. R., & Stević, T. (2008). Anti-inflammatory, gastroprotective, free-radical-scavenging, and antimicrobial activities of hawthorn berries ethanol extract. Journal of agricultural and food chemistry, 56(17), 7700–7709. https://doi.org/10.1021/jf801668c
Dağlı, Ü., & Kalkan, İ. H. (2017). Treatment of reflux disease during pregnancy and lactation. The Turkish journal of gastroenterology : the official journal of Turkish Society of Gastroenterology, 28(Suppl 1), S53–S56. https://doi.org/10.5152/tjg.2017.14
Ali, R., Hassan, J., & Egan, L. J. (2022). Review of recent evidence on the management of heartburn in pregnant and breastfeeding women. BMC gastroenterology, 22(1), 219. https://doi.org/10.1186/s12876-022-02287-w
Vazquez J. C. (2015). Heartburn in pregnancy. BMJ clinical evidence, 2015, 1411.
Thélin, C. S., & Richter, J. E. (2020). Review article: the management of heartburn during pregnancy and lactation. Alimentary pharmacology & therapeutics, 51(4), 421–434. https://doi.org/10.1111/apt.15611
Phupong, V., & Hanprasertpong, T. (2015). Interventions for heartburn in pregnancy. The Cochrane database of systematic reviews, 2015(9), CD011379. https://doi.org/10.1002/14651858.CD011379.pub2
Peterson C. (2012). A case study of chiropractic management of pregnancy-related heartburn with postulated fetal epigenome implications. Explore (New York, N.Y.), 8(5), 304–308. https://doi.org/10.1016/j.explore.2012.06.001
Thomas, M., & Weisman, S. M. (2006). Calcium supplementation during pregnancy and lactation: effects on the mother and the fetus. American journal of obstetrics and gynecology, 194(4), 937–945. https://doi.org/10.1016/j.ajog.2005.05.032
Mungan, Z., & Pınarbaşı Şimşek, B. (2017). Which drugs are risk factors for the development of gastroesophageal reflux disease?. The Turkish journal of gastroenterology : the official journal of Turkish Society of Gastroenterology, 28(Suppl 1), S38–S43. https://doi.org/10.5152/tjg.2017.11
Voropaiev, M., & Nock, D. (2021). Onset of acid-neutralizing action of a calcium/magnesium carbonate-based antacid using an artificial stomach model: an in vitro evaluation. BMC gastroenterology, 21(1), 112. https://doi.org/10.1186/s12876-021-01687-8
Garg, V., Narang, P., & Taneja, R. (2022). Antacids revisited: review on contemporary facts and relevance for self-management. The Journal of international medical research, 50(3), 3000605221086457. https://doi.org/10.1177/03000605221086457
Lee, J. A., Shin, M. R., Kim, M. J., Lee, J. H., Park, H. J., & Roh, S. S. (2021). Protective Effects of Inflammation of Curcumae Longae Rhizoma 30% EtOH Extract on Acute Reflux Esophagitis Rats. BioMed research international, 2021, 8854945. https://doi.org/10.1155/2021/8854945
Li, Y., Chen, Y., & Sun-Waterhouse, D. (2022). The potential of dandelion in the fight against gastrointestinal diseases: A review. Journal of ethnopharmacology, 293, 115272. https://doi.org/10.1016/j.jep.2022.115272
Haniadka, R., Saldanha, E., Sunita, V., Palatty, P. L., Fayad, R., & Baliga, M. S. (2013). A review of the gastroprotective effects of ginger (Zingiber officinale Roscoe). Food & function, 4(6), 845–855. https://doi.org/10.1039/c3fo30337c
Ramya, R. S., Jayanthi, N., Alexander, P. C., Vijaya, S., & Jayanthi, V. (2015). Gastroesophageal reflux disease in pregnancy: a longitudinal study. Tropical Gastroenterology, 35(3), 168-172.
Tsou, V. M., Young, R. M., Hart, M. H., & Vanderhoof, J. A. (1991). Elevated plasma aluminum levels in normal infants receiving antacids containing aluminum. Pediatrics, 87(2), 148–151.
Mulder, B., Schuiling-Veninga, C. C., Bos, J. H., de Vries, T. W., & Hak, E. (2013). Acid-suppressive drug use in pregnancy and the toddler’s asthma risk: a crossover, case-control study. The Journal of allergy and clinical immunology, 132(6), 1438–1440. https://doi.org/10.1016/j.jaci.2013.07.012
Charpiat, B., Bleyzac, N., & Tod, M. (2020). Proton Pump Inhibitors are Risk Factors for Viral Infections: Even for COVID-19?. Clinical drug investigation, 40(10), 897–899. https://doi.org/10.1007/s40261-020-00963-x
Uwaezuoke, S. N., Ayuk, A. C., Eze, J. N., Odimegwu, C. L., Ndiokwelu, C. O., & Eze, I. C. (2022). Postnatal probiotic supplementation can prevent and optimize treatment of childhood asthma and atopic disorders: A systematic review of randomized controlled trials. Frontiers in pediatrics, 10, 956141. https://doi.org/10.3389/fped.2022.956141
Alam, M. J., Xie, L., Yap, Y. A., Marques, F. Z., & Robert, R. (2022). Manipulating Microbiota to Treat Atopic Dermatitis: Functions and Therapies. Pathogens (Basel, Switzerland), 11(6), 642. https://doi.org/10.3390/pathogens11060642
Linder, L., Tamboue, C., & Clements, J. N. (2017). Drug-Induced Vitamin B12 Deficiency: A Focus on Proton Pump Inhibitors and Histamine-2 Antagonists. Journal of pharmacy practice, 30(6), 639–642. https://doi.org/10.1177/0897190016663092







