It’s no surprise to say allergies and asthma have skyrocketed in kiddos over the past few decades. Sadly, we can give some of the blame to vaccines. I promise to connect the dots for you, but first a quick lesson (and important one) in immunology before diving into the meat of this piece.
Our immune system, besides being totally awesome, houses 2 types of helper cells- TH1 and TH2. These Helper T Cells are arguably the most important cells in adaptive immunity, and without them, we cannot defend ourselves against even microbes (bugs) that are normally harmless.
- TH1 cells primarily kill viruses, bacteria, tumors, and other foreign microbes that try to invade our body.
- TH2 cells primarily protect our body from external allergens and chemicals in the environment (nerds can continue learning here).
Stay with me, I promise this is worth it.
In walk TH1/TH2 and the Hygiene Hypothesis
When a fetus is in the womb, its little immune system is TH2 dominant, and good thing, so mom’s own immune system’s TH1 cells don’t attack the fetus, thinking it’s a foreign invader. During delivery when being pushed through the birth canal, babe picks up microbes from mom’s genital tract (18 species) and fecal flora (about 400 species). When babe starts nursing, 8 more species of microbes are picked up. [1] At this point a shift in babe’s immune system from TH2 dominance to TH2/TH1 balance begins to occur.
Hang with me, it’s getting good.
It’s imperative the shift from TH2 to TH2/TH1 happens, and the quicker the shift happens, the better and here’s why:
TH2 dominant immune systems suffer from things like allergies, atopic eczema, and hay fever. And it’s worth mentioning several cancers, as well as post-operative infections, have been linked to TH2 dominance. [ 2, 3, 4, 5]
There’s a great meta-analysis that shows “20% increase in the subsequent risk of asthma (under the hygiene hypothesis) in children who had been delivered by caesarean section.” [6] These kiddos didn’t get to take the trip down microbe alley, subsequently their TH2 is still dominant.
In walk Vaccines
Guess what else can push TH2 dominance? Well, not vaccines per se, but the aluminum (and mercury), an adjuvent in vaccines, does. (Side-note: Aluminum is also linked to many neurodegenerative diseases, but that’s another story for another day. [7])
I like the way this scientist puts it, very eloquently:
“One possible contributing factor to the increase in allergies in the west is that the most commonly used adjuvant for vaccines in humans aluminum hydroxide is also a known Th2 inducer in mice and humans, so understanding its mechanism of action might have great implications for design of better adjuvants.” [8]
Oh good! I’m happy to know science knows we need to fix this?? Aghhhhhhh!!!! (sorry, had to pull my hair a sec.)
Here’s another good piece of research:
“Although aluminum based adjuvants are effective in certain vaccine formulations, they elicit mainly a TH2 response..”
Further…
“…the addition of adjuvants like alum to vaccine formulations can stimulate IL-10 production, leading to the suppression of a TH1 response.“
And in conclusion..
“Aluminum based vaccines may also cause unwanted side effects such as local reactions, augmentation of IgE antibody responses and granulomas.” [9]
PS. “Augmentation of IgE antibody responses” is a scientific way of saying “allergic reactions.”
Basically in a nut shell….
Science understands that using aluminum in vaccines drives a TH2 response in humans, and is most likely a major problem regarding the dramatic increase in allergies in America.
One of our heroes in the know, Paul Offit, MD states:
“…infants receive about 4.4 milligrams of aluminum in the first six months of life from vaccines.”
You can find the vaccines that contain aluminum, here. PS. The hepatitis B vaccine (given at birth) is one of them.
So, if we think aluminum in vaccines is a bad idea (for good reasons as stated above), here’s how we can protect our children….
In walks Passive Immunity
I bet your child’s pediatrician didn’t even tell you about this. You can safely withhold vaccination of certain “vaccine preventable diseases” via mama’s awesomeness for up to a year…
Passive immunity occurs when antibodies from one person are passed on to another person. The most common form of passive immunity is the antibodies against “vaccine preventable diseases” an infant receives from its mother. Our hero in the know, the CDC, explains it best:
“Antibodies are transported across the placenta during the last 1–2 months of pregnancy. As a result, a full-term infant will have the same antibodies as its mother. These antibodies will protect the infant from certain diseases for up to a year. Protection is better against some diseases (e.g., measles, rubella, tetanus) than others (e.g., polio, pertussis).”
There are a few points to understand regarding the above statement:
- For Hib disease, maternal antibodies generally provide protection for the first 6 months of life. [10]
- Full term babies will acquire more passive immunity than those born prematurely, so the longer the bun can remain in the oven, the better. [10, 11, 12]
- Studies show passive immunity can occur as early as 18 weeks gestation, so premature babies will still acquire passive immunity, the immunity just won’t last as long. [13]
- If the mother acquired the disease naturally in her lifetime as opposed to being vaccinated for it (like us having chickenpox as a kid), more immunity is passed on to her child.
- Here’s the kicker: When maternal antibodies are elevated in a child (during the first year), vaccines don’t work as well, and the “booster” is needed. So if children are vaccinated when maternal antibodies are gone, less vaccines in a series are needed because the vaccines will be more effective. [14, 15] Did you get that? You can give less shots, and they’ll be more effective. Also, the longer you’re able to wait to vaccinate your child against diseases like Hib and pneumococcal, the less doses they’ll require anyway, says the CDC vaccine schedule. Amen to that!
Another thought regarding passive immunity:
If you’re concerned about your child catching a “vaccine preventable” disease, but you’re also concerned about vaccinating them, I always suggest to my female patients they can have their titres tested to make sure they’ll confer passive immunity. If titers are low, get vaccinated themselves one year prior to conception to pass the antibodies to their child (the science says get vaccinated during pregnancy- tetanus, influenza, and pertussis, and soon RSV and group B strep, but I’m not on board with that yet). [16]
In walks Breastfeeding
On top of the maternal transfer of antibodies in the womb, you can also transfer passive immunity protection through antibodies in breast milk. [17] Breast milk is like “gold” for the immune system, not only to help with nutrition and gut development, but for the maturation of the immune system. [18, 19]
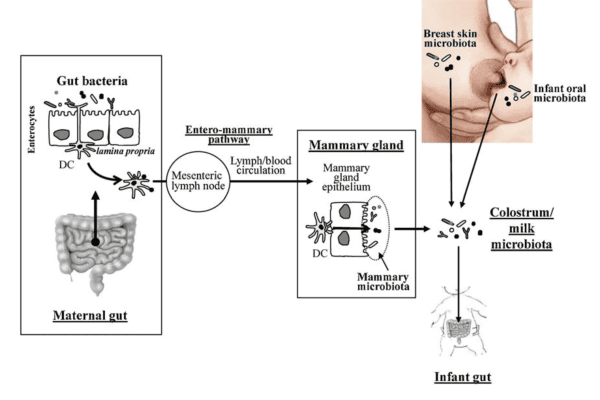
(photo courtesy of http://blogs.scientificamerican.com/WSS/post.php?blog=23&post=1343)
Here’s a handy chart to see what exactly is in breast milk.
Research released recently shows breast milk is nature’s perfect instigator of the TH2 switch:
“Breast milk stimulates the proliferation of a well-balanced and diverse microbiota, which initially influences a switch from an intrauterine TH2 predominant to a TH1/TH2 balanced response and with activation of T-regulatory cells by breast milk-stimulated specific organisms (Bifidobacteria, Lactobacillus, and Bacteroides).” [20]
And since we’re covering the vaccine topic, breastfeeding is protective against Hib, pneumococci, polio, rotavirus, measles, mumps, and rubella. [21]
I’ll leave you with this piece of research:
“Haemophilus influenzae is the major cause of otitis media and lower respiratory tract infection in childhood.” ……”The results suggest that the colonization of H. influenzae in the throat was inhibited by the presence of breast milk.” [22]
(Side-note: For those of you who may not be familiar with Haemophilus influenzae, it’s the long way of saying “Hib,” one of the diseases that we vaccinate against, 4 doses to be exact.)
Yay for breast milk! Not only does it help transfer passive immunity from mother to child, but breast milk also helps to decrease the likelihood of asthma and allergies by instigating a switch from TH2 to TH2/TH1 balance!
Other factors to consider
There are other factors to consider when deciding whether to postpone vaccinating your child (or perhaps not vaccinating at all). For instance, your child’s nutritional status, any known diseases or allergies, smokers in the house, older/younger siblings in the home, race, plans to travel, etc can really make a difference. It’s most important to sit down with your doctor and go over everything prior to making any decisions.
There’s so much science out there to thumb through, so continue educating yourself. At the end of the day, the greatest parents are the informed ones. I’d love to hear your thoughts! All comments, positive and negative, keep me on my toes! 🙂
(Disclaimer: Scientific information presented in this article is for educational purposes only and does not constitute medical advice on vaccination.)
Resources:
Immunisation Advisory Center- NZ: http://www.immune.org.nz/faqs/how-many-germsantigens-baby-exposed-birth
Kidd, P. Th1/Th2 balance: the hypothesis, its limitations, and implications for health and disease. Altern Med Rev. 2003 Aug;8(3):223-46.
Lubega, J. T-helper 1 versus T-helper 2 lymphocyte immunodysregulation is the central factor in genesis of Burkitt lymphoma: hypothesis. Infect Agent Cancer. 2007 May 17;2:10.
Schmitz-Winnenthal FH, Volk C, Z’graggen K, Galindo L, Nummer D, Ziouta Y, Bucur M, Weitz J, Schirrmacher V, Büchler MW, Beckhove P. High frequencies of functional tumor-reactive T cells in bone marrow and blood of pancreatic cancer patients. Cancer Res. 2005 Nov 1;65(21):10079-87.
Matsuda A, Furukawa K, Suzuki H, Kan H, Tsuruta H, Matsumoto S, Shinji S, Tajiri T. Does impaired TH1/TH2 balance cause postoperative infectious complications in colorectal cancer surgery? J Surg Res. 2007 May 1;139(1):15-21. Epub 2007 Feb 9.
Thavagnanam S, et al. A meta-analysis of the association between Caesarean section and childhood asthma. Clin. And Exper. Allergy. 2007.
Exley C. Why industry propaganda and political interference cannot disguise the inevitable role played by human exposure to aluminum in neurodegenerative diseases, including Alzheimer’s disease. Front Neurol. 2014 Oct 27;5:212. doi: 10.3389/fneur.2014.00212. eCollection 2014.
Kool M, Hammad H, Lambrecht BN. Cellular networks controlling Th2 polarization in allergy and immunity. F1000 Biology Reports 2012;4:6. doi:10.3410/B4-6.
9Dong JC, Kobinger GP. Hypothesis driven development of new adjuvants: Short peptides as immunomodulators. Human Vaccines & Immunotherapeutics2013;9(4):808-811. doi:10.4161/hv.22972.
1Simister NE. Placental transport of immunoglobulin G. Vaccine. 2003 Jul 28;21(24):3365-9.
Ozbek S1, Vural M, Tastan Y, Kahraman I, Perk Y, Ilter O. Passive immunity of premature infants against measles during early infancy. Acta Paediatr. 1999 Nov;88(11):1254-7.
Leineweber B, Grote V, Schaad UB, Heininger U. Transplacentally acquired immunoglobulin G antibodies against measles, mumps, rubella and varicella-zoster virus in preterm and full term newborns. Pediatr Infect Dis J. 2004 Apr;23(4):361-3.
Israel EJ, Simister N, Freiberg E, Caplan A, Walker WA. Immunoglobulin G binding sites on the human foetal intestine: a possible mechanism for the passive transfer of immunity from mother to infant. Immunology 1993;79(1):77-81.
Sato H, Albrecht P, Reynolds DW, Stagno S, Ennis FA. Transfer of measles, mumps, and rubella antibodies from mother to infant. Its effect on measles, mumps, and rubella immunization. Am J Dis Child. 1979 Dec;133(12):1240-3.
Redd SC, King GE, Heath JL, Forghani B, Bellini WJ, Markowitz LE. Comparison of vaccination with measles-mumps-rubella vaccine at 9, 12, and 15 months of age. J Infect Dis. 2004 May 1;189 Suppl 1:S116-22.
Lindsey B1, Kampmann B, Jones C. Maternal immunization as a strategy to decrease susceptibility to infection in newborn infants. Curr Opin Infect Dis. 2013 Jun;26(3):248-53.
Hanson LA, Hahn-Zoric M, Berndes M, Ashraf R, Herias V, Jalil F, Bhutta TI, Laeeq A, Mattsby-Baltzer I. Breast feeding: overview and breast milk immunology. Acta Paediatr Jpn. 1994 Oct;36(5):557-61.
Grönlund MM, Gueimonde M, Laitinen K, Kociubinski G, Grönroos T, Salminen S, Isolauri E. Maternal breast-milk and intestinal bifidobacteria guide the compositional development of the Bifidobacterium microbiota in infants at risk of allergic disease. Clin Exp Allergy. 2007 Dec;37(12):1764-72. Epub 2007 Oct 16.
Field CJ. The immunological components of human milk and their effect on immune development in infants. J Nutr. 2005 Jan;135(1):1-4. (full text)
Walker WA, Iyengar RS. Breast milk, microbiota, and intestinal immune homeostasis. Pediatr Res. 2014 Oct 13. doi: 10.1038/pr.2014.160.
Oddy WH. Breastfeeding protects against illness and infection in infants and children: a review of the evidence. Breastfeed Rev. 2001 Jul;9(2):11-8.
Hokama T, Sakamoto R, Yara A, Asato Y, Takamine F, Itokazu K. Incidence of Haemophilus influenzae in the throats of healthy infants with different feeding methods. Pediatr Int. 1999 Jun;41(3):277-80.