Eczema (also called atopic dermatitis) is one of the most common chronic skin conditions in children. If your child struggles with itchy, inflamed, or irritated skin, you’ve probably heard of (or been prescribed) topical steroid creams. But many parents feel unsure about using them: Are they safe? Will they thin my child’s skin? Should we only use them as a last resort?
In this article, I’ll walk you through what steroid creams are, when they can be helpful, potential risks to be aware of, and ways to support your child’s skin more holistically, so you can make confident informed choices for your family.
What Are Steroid Creams?
Topical steroid creams (also called topical corticosteroids) are anti-inflammatory medications that you apply directly to the skin. They work by calming inflammation, reducing itching, and helping repair the skin barrier. But like all medications, they come with risks.
There are many types of steroid creams, ranging from mild (like hydrocortisone 1%) to potent (like clobetasol propionate). Your child’s doctor will usually recommend a lower-strength steroid for younger children or for sensitive areas like the face or skin folds.

When Might Steroid Creams Be Helpful?
For many children, eczema comes and goes, sometimes staying calm for weeks or months, and sometimes flaring with dry weather, heat, allergens, or stress. Steroid creams are sometimes used during active flares to:
- Calm intense inflammation and itching
- Allow the skin a chance to heal
- Prevent infection caused by scratching
In moderate to severe cases, steroid creams can bring fast relief when other home care techniques aren’t working. They can also give you and your child a break from the discomfort that constant itching brings.
Need tips for managing itchy skin? You may like this article: How To Use Oatmeal Baths For Soothing Itchy Skin
That said, steroid creams are not a long-term solution for preventing eczema or addressing the root causes of flare-ups.
To learn more about eczema, read this article: Eczema Treatment 101
Are Steroid Creams Safe for Kids?
When used sparingly and correctly (at the right strength, for the right amount of time, and on the right areas of skin) many children with moderate to severe eczema might feel better when using short courses of steroid creams during active flares.
That said, it is important to understand that these are not benign creams—they are medications that affect immune and hormonal pathways in the skin (and, in rare cases, the body). Like any medication, they carry risks. The key is informed, careful use.
If you’re looking for a doctor who can help you weigh your options, this list may help: Find a Doctor
Most Common Risks of Steroid Creams
Here are some of the most common risks parents should be aware of, especially with frequent or long-term use.
- Skin thinning (atrophy)
This is the most well-known risk of steroid creams, especially with prolonged or frequent use (1). Steroids can thin the skin by decreasing collagen and elastin production, making it fragile, translucent, and more prone to tearing. Skin folds (elbows, behind knees, groin, armpits), the face, and neck tend to be particularly susceptible. - Stretch marks (striae)
Thinned skin is more likely to develop stretch marks. These are permanent changes to the skin that do not resolve even when the steroid is stopped (2). - Changes in skin pigmentation
Some children develop lighter (hypopigmented) or darker (hyperpigmented) patches where steroid creams have been used (2). This can be distressing, especially on visible areas like the face. - Delayed wound healing
The anti-inflammatory effects of steroids can impair the normal healing response, causing cuts or scrapes in treated areas to heal more slowly and potentially allowing more opportunity for infection to take hold (3). - Increased risk of skin infections
Steroids suppress local immune function in the skin. This can make bacterial, viral, and fungal infections more likely in treated areas (4).
Less Common Serious Risks
Although less common, especially when steroid creams are used correctly under medical supervision, there are some more serious risks to be aware of. These tend to occur with higher potency creams, frequent use, or use over large areas of the body.
- Systemic absorption and hormonal effects
Though rare, especially in children using low-potency steroids correctly, it is possible for steroids applied to large surface areas or used frequently to be absorbed into the bloodstream. This can cause suppression of the body’s natural cortisol production (hypothalamic-pituitary-adrenal axis suppression), in effect, creating a form of internal steroid overdose (5). Signs can include poor growth, fatigue, irritability, and other hormonal imbalances. - Topical steroid addiction and withdrawal (TSW)
This is a controversial and not fully understood phenomenon that is being increasingly recognized, particularly in cases of long-term or inappropriate steroid use. Children (and adults) who have used steroids frequently may develop red, burning, inflamed skin that worsens when steroids are stopped, creating a vicious cycle (6).This condition is rare in children who are treated conservatively under medical supervision, but this risk underscores the importance of not using steroid creams chronically and of tapering use appropriately when needed.

Topical Steroids Have a Cumulative Effect Over Time
It is important to note that many of the risks noted above are dose- and time-dependent, meaning they become more likely the longer and more often steroids are used. A brief 5-7 day course of a low-potency steroid is unlikely to cause harm in most children. But regular, prolonged use, even of “mild” steroids, can add up over months or years.
Certain parts of the body absorb more steroid than others and thus carry higher risks:
- Face (especially around the eyes and mouth)
- Neck
- Genital area
- Skin folds (groin, armpits, elbows, behind knees)
In these areas, even mild steroids should be used very sparingly and with medical guidance. Many dermatologists recommend trying barrier repair strategies first and reserving steroids only for short courses when absolutely necessary.
How To Use Steroid Creams Safely in Kids
Here are some important tips if your child’s doctor recommends a steroid cream:
- Follow your doctor’s instructions carefully. Use the strength and duration recommended.
- Use the “fingertip unit” method to apply. A pea-sized amount is usually enough for a large area; applying too much doesn’t make it more effective and may increase risk of side effects.
- Avoid using strong steroids on the face or sensitive areas unless specifically directed. These areas are more prone to skin thinning.
- Don’t use steroid creams preventatively. They are meant to treat flares, not for daily maintenance.
- Take breaks. Give the skin time to recover between courses of steroids.
If you’re unsure about how to use the cream or if you’re worried about side effects, always check with your child’s doctor or dermatologist.

Supporting Your Child’s Eczema-Prone Skin Holistically
Long-term, your goal should be to strengthen and support your child’s skin barrier and gut health so flares happen less often and are less severe.
Here are some ways to do that:
- Moisturize generously and often. Thick creams and salves help lock in moisture and protect the skin. It is important to choose clean products without irritants. Apply at least twice a day and always after bathing.
- Identify and avoid triggers. Common triggers include certain soaps or detergents, food sensitivities, environmental allergens, heat, and stress.
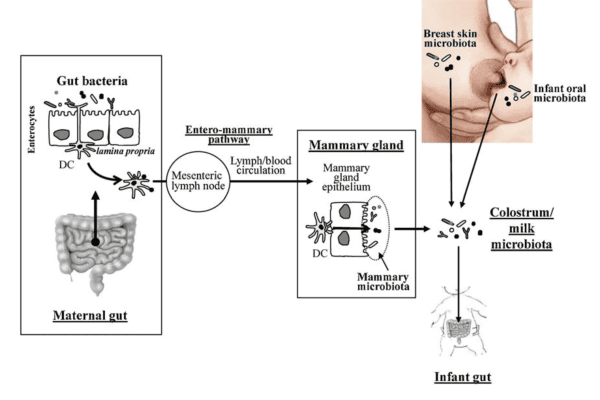
- Consider gut and immune support. There is growing evidence that the gut microbiome and immune function play a role in eczema. Probiotics, omega-3 fatty acids, and addressing food sensitivities may help.
- Support skin health nutritionally. Nutrients like vitamin D, zinc, and vitamin A are important for skin repair and immune balance.
- Use gentle skin care. Choose non-toxic, fragrance-free soaps and laundry products, and avoid irritating fabrics like wool.
If you’d like to explore a more integrative approach to eczema management, read this in-depth article: Eczema Treatment 101
Summary
Steroid creams can be a short-term tool for managing eczema flares in children, but they’re not without risk. Long-term use or frequent application, even of low-potency options, can lead to side effects like skin thinning and increased susceptibility to infection. When used correctly and sparingly under medical supervision, they can provide relief while the skin heals. For lasting improvement, it’s important to focus on supporting the skin barrier, reducing inflammation triggers, and nourishing your child’s body from the inside out.
References:
- Ricardo JW, Gosch M, Wang Y, Wright DN, Jorizzo J. Risk of skin atrophy induced by short-term topical corticosteroid use in atopic dermatitis lesional skin: A systematic review. JAAD Int. 2023 Jun 7;12:165-167. doi: 10.1016/j.jdin.2023.05.012. PMID: 37456622; PMCID: PMC10338287.
- Lax SJ, Harvey J, Axon E, Howells L, Santer M, Ridd MJ, Lawton S, Langan S, Roberts A, Ahmed A, Muller I, Ming LC, Panda S, Chernyshov P, Carter B, Williams HC, Thomas KS, Chalmers JR. Strategies for using topical corticosteroids in children and adults with eczema. Cochrane Database Syst Rev. 2022 Mar 11;3(3):CD013356. doi: 10.1002/14651858.CD013356.pub2. PMID: 35275399; PMCID: PMC8916090.
- Hengge UR, Ruzicka T, Schwartz RA, Cork MJ. Adverse effects of topical glucocorticosteroids. J Am Acad Dermatol. 2006 Jan;54(1):1-15; quiz 16-8. doi: 10.1016/j.jaad.2005.01.010. PMID: 16384751.
- Wong VK, Della Croce C, Schonfeld S, Mastrangelo AM, Lebwohl M. Use and abuse of topical corticosteroids in infections of the skin and related structures. J Drugs Dermatol. 2003 Jun;2(3):268-76. PMID: 12848111.
- Wood Heickman LK, Davallow Ghajar L, Conaway M, Rogol AD. Evaluation of Hypothalamic-Pituitary-Adrenal Axis Suppression following Cutaneous Use of Topical Corticosteroids in Children: A Meta-Analysis. Horm Res Paediatr. 2018;89(6):389-396. doi: 10.1159/000489125. Epub 2018 Jun 13. PMID: 29898449.
- Maskey AR, Sasaki A, Sargen M, Kennedy M, Tiwari RK, Geliebter J, Safai B, Li XM. Breaking the cycle: a comprehensive exploration of topical steroid addiction and withdrawal. Front Allergy. 2025 Mar 31;6:1547923. doi: 10.3389/falgy.2025.1547923. PMID: 40230788; PMCID: PMC11994697.